Are you or your patient a chronic muscle clencher? It may very well be the main cause of your tiredness, your many aches and pains, and speculatively even your high blood pressure. Unable to calm your body down? Keep on reading to learn how to identify and abolish this woeful muscle activation strategy, responsible for many maladies.
I have wanted to write this article for some time, but I did not, and honestly still do not know how to adequately explain nor phrase this very diffuse and – to my knowledge – unknown issue. However, I consider this issue so important, even vital, to general health, that I have to give it my best shot.
Be warned that this article is not going to be very scientific, because there’s no science on this topic as far as I am concerned. I haven’t really heard anyone discuss this topic in detail at all, which is why I feel the need to do so. You should know that this article is purely based on my own personal experience, treating chronic illness, and especially so after learning and using manual muscle testing (MMT) in my practice. Identifying clenching strategies is difficult, as the pattern is not unique and is often performed in a subtle manner.
Discovering this fundamental neuromuscular problem has also forced me to somewhat tone down my opposing views on the psychosocial theory of pain. I’ll talk more about that soon enough. So, without further ado;
What is “clenching”?
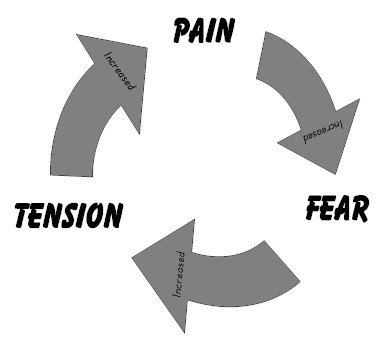
A “Clenching”-strategy is a person’s involuntary, excessive muscle activation strategy. The person is not able to exert force without coactivating and clenching improperly many muscles, and is not able to do so at a lighter force. It’s all, or nothing. ALL THE TIME.
Actually, there are three types of clenching. Two are bad including one being worse, and one is relatively harmless as long as it’s under control.
- Clenching as a strategy to brace or force-stabilize an injured or unstable structure
- Involuntary, constant global clenching
- Voluntary clenching, i.e competitive mind-set
Let me address these individually, and then I’ll discuss the solution.
Protective clenching / bracing
Whether it is a knee, shoulder, hip, neck or whatever else that happens to be injured, pushing through the pain will almost always create a bracing response to cope with the pain and instability. E.g, a person clenches all of the leg’s muscles every time he loads the leg that has a bad knee. If the pain is long-lasting, this strategy will not always go away on its own, especially if the person has been pushing through a lot of pain to cope with everyday life.
The bracing is somewhat beneficial because it helps to cope with the stressor; the instability and pain. In opposition, after the acute phase of the injury, the pattern of bracing will often not cease on its own. This exacerbates any muscular imbalances that are already present, because bracing an entire limb reflexively will imbalance normal muscle activation patterns, leading to uneven stimulus of the affected structures.
Such a person may go to a therapist and will be prescribed exercises to deal with the injury. Let us look at an example: A common driver of hip pain, is weakness of the deep six hip rotators. A therapist may identify this and prescribe strengthening of these muscles, for example by performing a clamshell exercise. For an ordinary, non-compensating patient this will stimulate the muscles well, it’ll feel weak and gradually the strength levels as well as muscle tone will increase. The hip will start to feel better.
For a strong compensating individual however, with a long history of pain in the given region, he is unlikely to be able to target these muscles without clenching the whole complex of muscles, maybe even the whole limb, or whole body. Firstly, this will greatly reduce the stimulus of the targeted muscles during the exercise, and because they’re being worked while simultaneously clenching a lot of synergistic structures, the likelihood of them being able to activate normally without compensation in daily life is very, very slim.
Therefore, such a strategy may severely reduce effectiveness of a form of therapy, even when the therapist was right in both diagnosis and prescribed the proper exercises. I learned this the hard way!
Corrective exercises for such patients must be very specific initially, and must be performed slowly without allowing the patient to clench the regional complex of musculature. Valsalva maneuver should also not be allowed, as it is as well a type of braing of the intrinsic core musculature. Hujing et al. 2003 as well as Stecco et al., has shown that between 30-40% of muscle force transmission passes through fascial connections, and if we study anatomy trains illustrations it will suddenly make a lot of sense why a person may attempt to clench their jaw, hold the breath or whatever else to increase their total strength. Although beneficial in situations where brutal strength is required, severe clenching strategies must not be allowed during rehabilitation.
Again, it’s fine to do this on a max 1RM squat, but it’s absolutely not fine when doing rehabilitative exercises or other simple exercises.
Global involuntary clenching strategies
A patient with a global involuntary clenching strategy (GICS), will be bracing their bodies, holding their breaths, clenching their jaws, and so on, for large portions of the day. Every single day. They are usually not able to exert moderate force with their muscles without bracing all of the body, and surely not without at least bracing the regional muscles, e.g hip complex. They are all or nothing; they aren’t able to exert resist a light pressure during MMT, nor a moderate pressure. They can, however, resist a high pressure, but only if they are allowed to brace the whole body.
This extreme muscle activating strategy is very taxing on the body. It is exhausting, and it creates massive muscle imbalances that do not resolve on their own, even when the patient rests more, exercises more, feels happier, feels sadder, it doesn’t really matter. The clenching persists and thus also its symptoms, although the severity of the symptoms will go up and down in relation to other factors, such as the before-mentioned.
These patients are often, sadly, the ones who often go from therapist to therapist with lots and lots of unresolved issues, all over the body. Their body may hurt everywhere, and they are often being told that it’s fibromyalgia or that it’s “all in their heads”, because the therapist can’t find sufficient signs and backing to explain these global aches and pains. They are often perceived as hypochondriacs. They often feel tired and exhausted, and may have shortness of breath. Such as person is extremely often a victim of global neuralgia, stemming from both brachial and lumbar plexus compression syndromes due to severe muscle imbalances, again stemming from their improper bracing strategy. The constant clenching will also cause more or less constant increase in intraabdominal pressure, something that may lead to pelvic floor dysfunction, reoccurring hemorrhoids, and so on.
When they talk, you can often see the platysma and infrahyoidal musculature pop out, like in the image highlighted in the beginning of this article. They may seem somewhat vigorous and stressed out when talking, no matter their current mood. Their movements are sometimes rough and quick. There’s a lack of balance in their movement patterns. This is by no means a complete list, nor should it be viewed as absolute – it is simply my best attempt of describing the signs of global clenching.
I have seen this strategy utilized by kids of 6 years old, ranging all the way up to adults of 70+. What seems to be a common ground, is a high toned personality, usually a person with slim body figure, high stress and/or worry levels, lots of responsibility, and so on. It may be business leaders, or someone who has been through trauma (such as violence, abuse, accidents), or someone with heavy metal toxicity (Read Amalgam Illness by Andrew Hall Cutler for more reliable information on this topic – it is a very controversial and poorly understood issue), or kids who have divorced parents, or people with difficult childhoods, and so on. I would say that the stronger the clenching strategy is, the more common it is to see more of the above mentioned traits, but of course, there are no absolutes.
If you are a patient of mine and you’re reading this article, please do not feel that I am trying to put you in a “group”, and surely do not feel that I am implying that all of the above-mentioned indicators applies to you. I DO NOT. I am merely trying to write down all statistical significant traits that I can think of, to help other therapists identify this dysfunctional neuromuscular strategy.
A person with GICS will usually respond poorly to high intensity exercise such as powerlifting, as it requires them to hold their breath and brace their bodies, exacerbating the existing dysfunction and its consequent imbalances. I have, ignorantly, done the mistake of prescribing valsalva-type training such as powerlifting to such clients in the past, only to realize that even though execution (technique) looks seemingly perfect, they were still getting injured. I really struggled with this for some time, but in the end I figured out why. They needed the opposite type of training; what we were already doing was harmful to them!
Proper exercise for a person with GICS is more of a moderate bodybuilding type of training regimen, where they should focus on muscle isolation, feeling the muscle work, and avoiding valsalva maneuvers and co-activation of whole muscle complexes. The exercises MUST be done slowly, because if they are allowed to go fast, they will clench. Bodybuilding training is also beneficial because it helps to tone the body and thus increases self esteem both for men and women. A double win!
A GICS patient will often require a tremendous amount of work and dedication to rid themselves of this strategy. It is extremely deeply rooted in their limbic system. Expect several months, maybe years, to completely let go. There will of course be dramatic improvements all along this way, so do not feel discouraged when reading these time aspects; it doesn’t really matter. Getting started and ceasing the clenching strategy is what matters!
Voluntary / competitive clenchers
This section probably isn’t all that enlightening, but it’s worth mentioning.
Some people are simply competitive, and clench purposely to obtain greater strength. If you are assessing such an individual with MMT or prescribing him corrective exercises, the results will be diminished by improper bracing strategies, as mentioned earlier. However, unlike the other groups, a voluntary clencher will easily be guided on how to properly perform the exercises as well as how to react to your MMT pressure. The competitive, voluntary type clencher is usually male.
The key here is awareness. Actually, awareness is the key for all of these groups, but the competitor-type individual will easily adapt to guidance and easily feel when they’re doing it right or wrong. If you ask them “did you clench your whole body?” they’ll confirm it and usually stop doing it on their own, if you let them know that it’s not appropriate.
How I first identified clenching strategies
I have touched on this already, and also in other articles, but after I started using MMT in my practice, I quickly discovered a relatively rigid pattern where muscles that were painful, also were weak. They could be tight, they could be big, they could be small, but they were virtually always weak. And, rehabilitating these muscles with proper exercises resolved the pain permanently in the great majority of occasions.
However, I had a few difficult patients where everything happened to be up-side down. The non-painful sides were weak, but the painful sides seemed strong. I scratched my head over this for several months. I tried to release those muscles, no results. I tried to strengthen them, no results. I simply could not help these patients with my then current approach!
Eventually as my therapeutic experience grew, these handful of patients were starting to really bother me. All my other patients were getting better, but these ones were marginally improving, if at all. I knew that the muscles were weak even though they seemed strong, although I didn’t understand why. The exercises they were using didn’t improve the condition at all. WHAT COULD BE THE PROBLEM?
It all changed when I got a patient whose compensation pattern, i.e his clenching strategy, was extremely obvious. I could literally see how he braced ALL of his body reflexively for just about anything. And this compensation was more obvious when testing weaker structures, yet less obvious on muscles that were functioning better and had a greater strength. This patient was very open about his emotional struggles, and fits with many of the traits I described above in the GICS section.
After this, I started noticing the same pattern in other, more subtle compensators. They were subtle clenchers! No wonder I had not discovered the compensation, because they were so good at this “cheating” strategy that no jerking movement could be observed what so ever. The only thing that separated these from a normal group, i.e a normal strong and functional muscle test, was that “something didn’t quite feel right” or “didn’t quite make sense”. Women are especially subtle and difficult to assess for this dysfunction. Even now, after I’ve worked with this for quite some time, I have to ask “did you clench your whole body?”, especially when assessing women, if something doesn’t quite add up.
GICS makes pain science make more sense
I strongly consider myself a “structuralist”, using logical mechanical approaches in my treatment approaches, as is evident in all other articles that I’ve written. Extremists within the psychososcial pain theory community claim that there is no correlation between structure and pain at all, which I consider to be utter nonsense. However, there are a lot of studies, especially statistical studies that show strong correlation between psychosocial factors and pain. Logically, all of these can’t just be made up – there has to be something to it. Maybe a golden middle way, or perhaps some important nuances?
Seeing a lot of different patients, and most of them having poor posture and issues correlating with this, I can truthfully say that posture is NOT what separates people with a lot of issues from those who do not. It is their clenching. People who clench a lot, in my experience, they get a lot of problems. Nerve pain seems to be the most common denominator for clenchers. Thoracic outlet syndrome, lumbar plexus compression syndrome, and similar “syndromes” are very prevalent in the GICS group. I am seeing 20 year-olds with global nerve pain issues. 20 year-olds! And even though they generally do have poor posture, other patients with the same postures or even worse postures, do not have the global maladies, often presented as nerve pain, as these patients do.
Therefore, I propose the notion that clenching syndromes may be the real culprit and cause of correlation between musculoskeletal problems, especially chronic ones, and the statistically significant psychosocial aspects that many studies are pointing out.
How to identify GICS and other clenching strategies
For now, the only way that I’ve managed to identify improper clenching strategies, and especially distinguishing between the different types, is by using muscle testing. Muscle testing is a skill and takes time to develop; and unfortunately the lacking concrete criteria of identifying GICS does not make it any easier. Detecting GICS and similar issues may therefore prove difficult for some, so don’t expect to identify these things without spending a lot of time doing MMTs on a great variety of people.
Either way, let me tell you how I do it: Let’s say a person has greater trochanter bursitis, which, for your information, is almost always caused by weakness of the tensor fascia latae muscle. So, the first natural thing to do would be to assess this muscle, for example with a muscle test. But, the test will falsely show that the muscle is very strong, due to bracing. Most therapists will then go on to release it, but we are NOT going to do that, because the likelihood of this muscle actually being strong and functional is close to zero if there’s trochanteric bursitis present. So we ask the patient: “are you clenching your whole body?”, most of the time they’ll admit that yes, they did, but sometimes they won’t.
You retry the test, and if it’s now weak, that could either mean that they don’t know how to NOT clench, or that they’re just not a GICS-type clencher. If it’s still super strong, ask them again to meet your pressure naturally. If they simply “get” what you’re saying, and calm down the clenching without much instruction, it’s probably just competitiveness. If this goes back and forth a few times, however, and the patient isn’t able to activate the muscle without clenching the whole body or regional complex, or nothing at all, then you can proceed to test other muscles unrelated to the injury. If the patient is able to perform elbow or shoulder flexion and extension, for example, without any clenching, then it’s probably a protective strategy that’s going on with the hip complex. If, however, the clenching persists instinctively no matter where you perform your muscle test, then this is most likely a GICS type patient.
If your patient presents with neuralgic issues that are seemingly not disc related, always consider GICS. I have not once seen a patient with lumbar plexus compression syndrome, for example, who did not have GICS. I have however, seen a couple of patients with thoracic outlet syndrome (articles addressing both issues are linked further up) who did not, due to the slightly more multifactoral nature of its aetiology (e.g clavicular depression in posture). That said, myofascial nerve entrapment (MFNE) syndromes such as the before-mentioned are the often epitome signs of GICS.
Unfortunately both GICS and MFNE are relatively difficult to diagnose and will be missed by most therapists, but it’s important to know about these things in order to gradually increase awareness with regards to its existence.
What to do about chronic muscle clenching
Chronic muscle clenching, especially GICS, is a significant dysfunction that mandates neuromuscular reconfiguration, to use such a term. I consider GICS (especially) so severe that it must be addressed and altered.
Awareness is the key.
Once the therapist (or, rare, patient him- or herself) has identified a clenching pattern, the patient will need to be aware of this when performing corrective exercises and whatever other situations where this may be important. This applies to GICS, competitiveness and to protective bracing strategies.
For GICS, however, the bracing doesn’t stop at exercises or similar issues. It’s constant. The patient has to be aware of their habit by first learning that they do it, and then how to not do it. This is done by performing muscle tests on them again and again and again until they’re able to attempt to resist your pressure naturally without clenching. I say attempt because they won’t be able to resist you, but they should be able to attempt it , and they should be able to distinguish somewhat between clenching and non-clenching resistance. In the beginning, they’ll have no clue that they are clenching, nor what they are supposed to feel, nor how not to clench. It takes a lot of repetitive work to get them to feel the difference, because this is the key. It takes a lot of work.
They can’t work on something they do not feel.
Once a GICS patient feels the difference between clenching and non clenching (it doesn’t matter whether they’re able to exert true force or not, at this point), they’ll be able to identify when they’re doing it in daily life, and thus also to stop it. They’ll feel weak, they’ll feel that they aren’t able to use their potential, but that’s fine. It takes time to get rid of a dysfunctional habit that’s been active for 10-20-30-40 years. Patience! Keep up the great work.
A little story
A friend came into my clinic with forearm pain. He also had a long history of other issues, such as hamstrings, back, shoulder, etc. He was very strong (deadlifting nearly 300 kgs / 660 lbs), and had been exercising for many years. But, he kept getting injured, continuously. Any other person would have stopped training for all the injuries, but not this stubborn guy. He had spent thousands of dollars on treatments prior to seeing me, to be able to keep training.
Anyway, this time it was forearm pain. I had treated him for other issues prior to this, but relatively good results, but as I said, there was always something more, or recurring. There was some time since I had seen him, actually, the last time was before I started noticing these clenching habits with other clients. Upon the visit, I finally noticed that he turned out to be a clencher as well; no big surprise, considering his extensive injury history. I told him that he was clenching and that this had to stop. He was surprised and a little doubtful – “I am not clenching”, he said. “At least I can not feel that I am doing it!”. I told him some stories of other people, that he seemed to be the same type, and that I wanted him to start paying attention to his clenching habits. We did some muscles tests back and forth until he started to feel what I was talking about.
By the way, this guy is very busy, runs several businesses and has lots of responsibility. A relatively common trait for GICS-ers.
About three weeks later he sent me an SMS. He told me that he had noticed how he, during daytime at his desk job, was clenching his quadriceps muscles CONSTANTLY throughout ALL THE DAY. He had never noticed this before. Later on, he noticed more and more patterns, and after this, I didn’t see him for an injury for a long time.
In summary
Chronic muscle clenching (syndrome?) is in my view quite a pathological habit. This applies especially to GICS; global involuntary clenching strategies, but may also apply to the lesser versions (protective clenching & competitive clenching) in the right circumstances, if undetected and unaddressed.
GICS often affects highly stressed or worrisome people, perhaps also those who has been through difficult situations in the past, and involves inability to exert force without clenching the whole body or a regional complex. Protective bracing, however, is usually developed as a strategy to cope with pain or instability. Competitive bracing is relatively self-explanatory, but it involves bracing the body in order to gain more strength, increasing the odds to “win” at whatever is being attempted.
The primary treatment for GICS and similar clenching strategies is awareness. The patient has to become aware of their habit, what it feels like doing it as well as not doing it, and then stop it whenever they notice it happening, especially in daily life. Powerlifting or similar high intensity training that promotes a lot of clenching and bracing, is not a great hobby for someone that struggles with GICS. They need slower, more careful exercising until they are able to greatly diminish their clenching habits.
Finally, clenching “syndromes” are something very diffuse and diffcult to pinpoint. Identifying this deeply rooted dysfunction was – without any doubt – a missing link in my treatment protocol, and a very important tool to have in the toolbox. It helped me to finally understand why some people were not responding to exercises and approaches that had great results on other patients with the same kind of complaints (e.g quadratus lumborum pain, which is a synergist in respiration). I truly believe that GICS is a huge driver of dysfunction, and I hope that this article, although somewhat obscure and esoteric, has shed some light on it as well as a provide a possible approach f0r identification and resolution.









Hi,
I have been following your articles for some time. I just found this one.
But I have a question.
If I am struggling with TOS or with Lumbar plexus neuralgia, in order to treat them , some bracing will be performed. Ether in thoracic or lumbar region . How to separate the good and the bad bracing? For example. When I am lying or standing I have to keep my chest up in order to stop the pain in my shoulder from TOS. The moment I stop , it start to hurt.
Thanks!
Wrong. No bracing during rehab.
Hi hello i always have to clench my muscles ,it gets on my nerves because my whole body always needs to feel the urge to clench and i twitch and its sore and numb,is there any way u can tell me what this is?
Apparently I am a clincher I do not do this to mask a pain it’s more on an emotional level. Whether I am excited about doing something, whether I am doing something completely different than normal, or even sitting down to do my hobbies like I used to do. My age is 67 and as I get older they get worse. I’ve had them on my life but have been able to hide it because I didn’t do it very often. Over the last 3 years they have gotten so bad that I cannot hardly control them. Not to mention the pain in my thoracic area of my spine. My clinches are my jaws my neck shoulders and thoracic part of my spine. I do however have a lot of pain in my spine now due to all of that clenching. I’m very excited to read about this because I’ve always called it nervous fits. I don’t know what doctor to go to and neurologist a hormonal or a spine doctor. I had migraine headaches for years and they always lasted 3 days on the left side of my head. But they went away probably 8 years ago. I just wondered if this could have anything to do with it. I guess I’m just asking for advice on where to go from here because they are getting so bad it’s cutting into my daily routine, and very noticeable by others now.
Hello. How do I get educated on GICS?! I just realized I do this myself (literally realized it 2 days ago) and I want to add this to my massage therapy practice. This article made me cry when I read it as I’ve been struggling with this for many, many years! The pain has really increased the last 3 years. Would like to find some classes near me, if possible.
I stumbled upon this article while searching for why my abs and quads are constantly clenched. I suffer with chronic back pain & developed this clench over time. My abs are strong from core strengthening exercises, but my legs are weak. I found help thru a PT gal that stretched my quads, glutes & back of legs. She has recommended belly breathing & wants me to be aware of the contraction of all my core muscles & try & relax them. What she doesn’t have an idea for, is back strengthening exercise that won’t cause more damage. Any recommendations from you would be great!
Does this have a relationship to Bruxism?
Probably.
What type of Dr/therapist should I see if I clench my inner thighs. I have a problem with my hamstrings, pelvic and hip flexor area also. It might be my jaw but sometimes I feel like Im clenching my brain muscle. It’s been like this for as long as I can remember. Thank you
Just stop clenching them. If you can’t, see a psychologist to find out why.
I relate to this comment. While awareness helps 50-60% of my day I am clenching and sometimes holding my breath. My pelvic floor is tight, thighs and jaw. My hands naturally are in fist especially while I sleep. I feel lost. I have been to PT for years and still am week.
I’m always tired. How do I find out more ways to help myself? What do I say to therapist to help me?
Thank you, thank you, thank you. A thousand times, thank you! This discovery is going to be life changing!! I just became aware that i was clenching, all the time, all day, everywhere.
Takk, det er veldig lærerikt å lese på denne nettsiden. Jeg har hatt en misstanke om og forsøkt å slutte med det du beskriver her. Jeg har det med å låse tungen i ganen, og har klart å redusere spenningen av muskler i resten av kroppen ganske bra, men det har tatt tid. Jeg spenner musklene fra hodet til skuldre, holdning er en stor faktor med instabil nakke og så er det spørsmålet om øvelser for trening av muskler som har vært vonde og i ulage siden 1988, ca to år etter bilulykke. Livet er en lang skolegang, lærer stadig nye ting om meg selv.
Bra jobba. Tungene skal “hvile” i ganen (altså oppe), men ikke presses mot ganen.
hi ı have been clenching my leg and hip muscles for a long time .and ı can’t quit this habit. every muscle of my lower body has a letter of alphabet . ı repeat peoples words with my muscles . It makes me improve my muscles incorrectly. it also make my hip muscles bigger( almost 3x bigger )ı still dont know how to get rid of that. but thank you so much for giving informations.
Give it some time. It takes time.
Consider simultaneous use of anxiolytics or simply giving yourself more rest.
Great article. I discovered I was a global clencher 20 years ago as I was on a relaxing stroll and was holding my umbrella so tight that my entire arm felt like it was going to fall off when I switched hands. 20 years on and I find as soon as I relax one set of muscles, it moves secretly somewhere else. It’s a very complex problem and I find as I relax my compulsively over-tensed muscles, the first experience is pain from letting go.
The muscles are so sore and so weak, a protective clenching resumes almost right away. It’s very tricky to wind it all down and perhaps only meditation is the answer. I don’t yet know. Thanks for figuring it out. I’ve tried to tell doctors, physios, dentists, oral-facial specialists and they all give you that same look.
This is exactly how I am! I’m 31, and discovered I clench all over all the time when I was about 18. For me, I’m certain it’s a trauma response from childhood.
The same thing happens to me when I discover that I’m clenching in one area, it moves on to another very sneakily. It is exhausting. I often wake up with unusually sore muscles – I think I clench a lot when I sleep.
I am also trying meditation, yoga, and breathing to help with it.
Good luck to you!
Kjetil great article! Have you had any results with myofascial release? This has been my main use for rehab, but after reading your article, I believe done intensely and without conscious thought can just causes more clenching throughout the body. Or are you just seeing results with the isolated muscle exercises?
Waste of time
This is exactly what I think is wrong with me- I have general anxiety disorder and involuntarily brace myself for stress and anxiety. It has lead to extreme neck- shoulder and back pain. I just didn’t have a band for it. Thank you for this article
I feel tension all over my body, and I am only aware of it when I get a massage, or even massage myself. It almost does not matter which part of the body, which muscle, all of them give me great relief when I have some pressure applied to them. It is like my whole body is in constant tension, 24/7.
I also have bruxism at night.
Does this sound like what you describe in your article? And what can I do about it? I am aware of the tension but cannot get rid of it.
Thanks for your help.
Yes.
Read the article a couple of more times. Also see my video on youtube.
I’m astounded I found this article! I injured my knee 18 months ago and started a journey of “ therapists”
I’m 53,slim and active. Have a physio I see weekly and do at least an hour exercises a day. My L Spine/SIJ/Hips and knee have me in tears some days. I am constantly squeezing all my lower body muscles even when I’m not aware of it.
Is this why I’m getting no better? Have I got to stop clenching? It seems natural now. I find it soothing.
And yes, my anxiety levels are through the roof with mild panic attacks.
can GICS significantly slow down muscle recovery (recovery from exercise)?
Probably.
Kjetil,
The GICS describes me completely – slim, stressed and constantly bracing. I have been dealing with certain pain syndrome for two decades. I can feel muscles are clenched by cant really do anything about it. Do you have ANY recommendations as far as who to talk to?
Thanks, I was not able to find anything about this problem on the Czech websites nor in english ones! I have that problem since I was a kid and sometimes I am really pissed of, but I felt that noone has the same problem and I am always thinking of telling this to my doc but then I feel like he would not even understand what is going on. And finally someone “named” it. Clenching of everything, bruxism, holding breath, thats my life, and it can be really annoying sometimes, I still was not able to stop it, in some periods of the year it is better and I feel so relaxed, when I finally know how to stop it at least for a short time. Yup it is hard to realize it and just stop, but I am glad that Im not that only one weird person in this world with this problem :D.
Extremely common problem
Reading this was very enlightening, I wonder if it has a connection with polyvagul theory. The constant clenching due to constant fight or flight being activated as a learned mechanism for basic functioning due to trauma.
Thank you so much Kjetil for such an eye-opening article. Reading this I realise I have nearly every single one of these symptoms that you describe and previously have just put it down to stress/anxiety/depression. I was diagnosed with hip osteoarthritis about 3 years ago (quite young to have it at 33).
I did use to do a lot of pole dance for fitness and other quite strenuous strength-based exercises but as the years have gone by the pain seems to be getting worse, not better, The last couple of years my low back pain has been getting worse with shooting sciatica now a regular occurance down my left side. I had been to an osteopath who just couldn’t get a diagnosis for me and in the end, it was suggested I just had a joint lock in my back.
The symptoms such as really bad circulation (always cold feet with pins and needles), reoccurring haemorrhoids (which the doctor just tells me is because of the pain medication for the osteoarthritis but even when trying not to take painkillers it still occurs), tiredness and pain which gets worse from activities such as getting in/out of cars/baths, household chores and washing the car for example.
I am becoming aware that I clench, and I clench ALOT. If I am bending washing the car I will be clenched so bad that to come out of the position is complete agony and can pretty much write off doing anything else for the rest of the day. I have also clenched my jaw so hard for a number of years but again the doctor said this was down to anxiety medication but again even when I’m not on the medication it still happens. Having read this makes me realise that this is a condition and now I think I can finally put a name to what I may be experiencing.
I had to write a comment as up until finding this article via a google search of my symptoms I had no idea this could be a problem let alone one that I could at least start becoming more aware of and start doing something about it so thank you.
Well done. This is the most common cause of non-specific chronic pain in the world, I believe.
Kjetil,
I can’t thank you enough for how validating it was to read this article. I have been the lost patient travelling from therapist to therapist looking for relief. I always felt I couldn’t activate the proper muscles for the exercises I was given to do at home and felt completely discouraged and hopeless for many years.
Over the last few years my awareness has grown and has indeed been the only relief of my pain, though the mental exhaustion of paying attention to when you are clenching or not is quite the stressful load as well. I notice a spike in my symptoms after a fight with my mother or any tough emotional experience. Esoteric or not, what you have written was a perfect description of what I live like every single day as someone with GICS (which I hadn’t ever heard of until this moment so thank you for allowing me to name this). And thank you for acknowledging the pain, confusion and exhaustion of experiencing this involuntary clenching. I was especially shocked at the accurate personality & physical description. People think I am so intense when I speak and I always thought I had to soften my tone but I realize I must actually soften my face as well. Thank you for bringing me even greater awareness & peace concerning this issue. Too bad there aren’t more committed professionals like you in Canada!
Wish you a speedy recovery!
I learned about this when I started eating mushrooms. And I was told “you didn’t go through puberty right.”
mushrooms helped a lot. they said “Imagine the body filling with golden light.” and “ sometimes it takes a while.“ well it’s been a year and a half and I’ve had great improvement. I also used an anal vibrator because the sphincter was almost impossible to loosen. it taught me how to sense that muscle.
My father is a CEO and I think the problem developed through my empathy and admiration for him. I wanted to be competitive and hard.
great article.
Great Article. Thank you for sharing, my Mum has been suffering from Peudendal neuralgia for 10 years. She’s had nerve blocks, pelvic floor treatments, therapies and so on but to now available. I believe her muscles have clench which is why she cannot get better. Any advise please.
The pudendal patients ALWAYS clench. Good catch
I am not from a medical or fitness background at all and have just stumbled across this article whilst searching the internet for answers as to why I always hurt and why I’m always so exhausted and reading it has made me cry in relief…I am a chronic clencher! And possibly a combination of each type that you mention.
I identified a while ago that I involuntarily clench my jaw, neck and shoulders during most things, especially when concentrating or hurrying, but even doing menial tasks like chopping onions or walking quickly! However, I can’t seem to do anything about it. If I notice it, I try to relax but either I physically can’t do the task without clenching or seconds later (I’m guessing here because I do it involuntarily) I’m clenched again! This has progressed over the years so that now it’s not just my upper body that is tense, but my buttocks and legs too, most of my active time, each and every day! It’s never been picked up by any therapist I’ve used: gp, physio, osteo, chiropractic, sports/deep tissue massage as a contributor to my discomfort (notice I dont say pain here as it’s not painful, more like fatigue and stiffness; like I’ve overdone a whole body workout).
I’d come to the conclusion that this is all due to anxiety, stress, low self esteem, hormonal tension, probably throw in some poor posture and definitely poor sleep (I often find that I’m clenching my whole body while trying to sleep) but trying to “fix” any of these things doesn’t seem to make any difference – I feel stuck in a cycle that perpetuates the problem but I just have to live with it. I have researched conditions such as fibromyalgia but the symptoms just don’t quite fit. I have adjusted my whole lifestyle over the past few years: cutting working hours, therapeutic exercise (yoga, swimming, walking), regular massage, acupuncture etc. and if anything, it’s getting worse!
Obviously I can’t be sure that this is 100% where my problems lie, but reading your article has been like an epiphany for me in understanding why I haven’t been able to make improvements to physical health thus far. I would obviously be interested to hear where/how you would recommend beginning the journey of retraining my body and mind! I am so very, very grateful that you did go ahead and write this article!
Hi Leanda,
Just read your response and can completely empathise with everything you are experiencing.
Would you be up for me contacting you directly? Would love to speak to someone who understands how I am feeling.
Feel free to contact me by email or Facebook messenger if you have it.
Kind regards, Kate x
Hi Kate , I’m a 48 year old male and I am often catching myself tending my leg and buttock muscles involuntarily. I am a runner . I run anywhere from 3 to 10 miles at a time . Back in march my legs felt exactly like miss foster described above . I had all kinds of blood work done and nothing was found . I have made some changes like adding some supplements and more protein but I still experience cycles of this , even after a few days rest , it makes no sense at all . Any help would be much appreciated.
I honestly feel like there should be a support group for this. because I also struggle with this
Make one
A Facebook group would be so beneficial as I believe this is exactly what I am experiencing. I can be sat on the sofa in the evening and happen to notice my whole body is tensed, I rlax and within minutes am tensed up again.
Leanda, try an anxiolytic drug. Talk to your GP or a psychiatrist.
Wow. This could be what I have. I’ve mentioned to several therapists, LMTs and NP that I find myself constantly, and I mean constantly, tensing up my legs and feet. I catch myself and try and relax but it happens again. Most of the time I don’t know I am doing this. Another weird thing I do is when I am sitting, my heel(s) are always up off the floor. Always. I never see anybody do it because I look around in waiting rooms etc. I also am a chronic leg shaker. I have been doing this for as long as I remember. It’s embarrassing because sometimes the shaking will rattle the table at dinner etc. I have just recently noticed that when I am taking a lid off a jar that is tight, I find myself clenching my teeth. Just like the picture above! Wow. Am I a mess or what? I have been in an extremely dysfunctional marriage involving gas lighting, indifference, lying, porn, alcohol and anger. I am trying to heal. Should I tell my therapists about this GICS? God Bless you. I think I finally have a name for this weirdness. Susan
whats the treatment of this?
I don’t know if this is the same, but I clench because I feel like when I lift my arm or place my body in a certain place my muscles some some what tickles \spasms to the point I need to apply pressure or bite my cheeks to stop the pain, I’ve had a mir scan and they’ve found nothing.
I’ve also read up about it being related to anxiety ocd, I don’t really know, I give up going to therapist to therapist, it honestly ruins my life, sometimes I can even make dinner for loved ones due to it, when I try to describe most people say ‘your muscles will be tired muscles from the gym or day’ when it’s just not that sort of pain, I’ve had it for years and would rather be told I had till 50 to live then live with this until 70.
Can anyone help please?
I think this is me. I’ve been obsessively trying to fix my posture for the last two years with no improvement. I ALWAY make that clenching face like the picture at the beginning when I do any type of physical exertion pretty much. I am always really intense and vigorous when conversing with people even in calm situations. I’ve been looking for answers everywhere and FINALLY I stumbled across this post. And now I can feel myself clenching all my muscles ALL the time. But I’m having a hard time unclenching. If I unclench one thing, I clench somewhere else. I honestly can’t keep living like this and I can’t find any more information on this. Is there any advice or anything you can give me? Im a 31 year old female and im so so so so tired of living like this. Im on edge all the time, My body is always exhausted , my posture is horrendous and I don’t know what to do anymore.
I been suffering from uncontrollable clenching, this keep happening while try to talk with my firend, when I’m alone it keep repeating without trying to clenching my jaw toward my teeth just like the first imagine i don’t know my doctor was unable to understand what going on, how can i stop it
Help…
Hello. I just wanted to thank you for this superusefull text. I was googling ‘how to stop clenching’ and found this comprehensive explanation about all the esthetical and other issues I’ve noticed about myself, but didn’t know how to address. Now with the whole picture, I’ll definitely approach it systematically and I can intuitively anticipate the whole spectrum of correlated improvements which is spreading as I keep writing this comment. Sorry, I got a little carried away, but I haven’t had this much of a discovery for a long time and I’m a constant digger for improvements. I’d also like to point out my disagreement with your modesty related to scientific results vs. professional’s like yourself. Scientific research is, in a sense, limited with it’s predetermined variables and questions, and a unique perspective as a result of cumulative focus you can give here is a huge contribution to overall understanding. Keep thriving and thanks again!
Thank you for this article. I am constantly clenching my entire body all day and night. My jaw hurts, my hips hurt, my arms hurt. It’s physically taking a toll on me. I don’t know what to do to correct it. I try to relax but I end up clenching harder. Please help
Try to stop clenching. It is normal to not have immediate results. If in one year, or maybe six months, it is not better, then seek help. Combination therapy of drug and counseling may be necessary.
Horrible, debilitating Pain Rt side neck pain (SCM) through upper trap and Rt scapula, since Summer ’20. Lots of major stress that year (other than pandemic) …(both parents passed w/in 1.5 yr of each other, sole caregiver for one for several months at the end, unexpected financial devastation, very complicated relationship issues, major move, hit mid-life (and menopause), devastating legal event that affected our family….. I have no doubt that psychological factors are affecting my physical state (TMS tension myositis syndrome) after seeing countless Drs. since 2020 w/ clear scans. Now Rt. pectoral, Rt ribs, Rt and Left occipital muscles with neck stiffness, both scapulas with pain etc. Stiffness, burning, deep aching. I now stretch my Rt leg and hip/glute and feel it up my back and in my neck (fascial?)…….and I always am clenched. Typing, reading, sitting, driving, standing…..even when I lie down at night, I find myself almost holding myself up and not relaxing completely into the bed or pillow….neck muscles tensing to the point where they often spasm at my SCM as I’m trying to go to sleep before I realize that I’m holding my muscles. I’m in a constant hypersensitized/flight/fight state. Painful and exhausting.
Same boat man. I’ve gotten lots of relief tho. Many modalities to explore, you really have to become obsessed with your health and make it your hobby at this point because in today’s society, healing is a virtue. I’ve found very good relief in spiritual/frequency based practices like sound bowl healing. Relaxing herbs like kava, Jamaican dogwood, crampbark. And therapies like myofascial release. I think most therapists would tell you stretching isn’t the best, and the generic google answer of “ decrease your stress levels” means nothing until you understand that this is a game of life and cannot be fixed with the easy button. Get yourself into a good mindset, your body will compensate greatly even if it doesn’t heal.
i believe that Feldenkrais as well as a comprehensive understanding of brain rewiring/training techniques and CPTSD therapy to be a useful combination. I took 2 years of alexander technique lessons and they truly helped me rewire my body. i did a weekend taster of feldenkrais and personally i found it better and more natural and sustainable than alexander technique. Currently i cannot afford either and my tensing has returned, particularly in the jaw. Meditating in ‘resting pose’ on the floor with my hips at 90 degrees, calves on a chair and meditating helps, as does most lying down floor work re re-educating the nervous system. I believe it is a form of dysautonomia. At least in the CPTSD cases.
Dear mskneurology.com administrator, Your posts are always well-balanced and objective.
Thank you for this article! I have been telling my husband for years that he exerts too much force for daily tasks and I think he is finally starting to believe me! He has broken countless brooms and mops and most recently our toilet flusher from pushing it down too hard too many times! He tells me when he lays down in bed, he feels himself forcing his head/body into the bed. When he sleeps, sometimes his hands are in fists. He is a fit 43 year old, 5″7′ man, very gentle man, so this is very strange to me! I recently told him to practice being “light as a feather” because we cannot figure out why he does this. He constantly has pain everywhere – mostly in his neck and shoulders – I wonder why! I started googling, and found this article. I am a therapist and have suggested therapy many times, but he does not see the correlation! I will keep encouraging it!
I am a 59 year old woman, I have suffered constant clenching issues for years… I have recently undergone lumber decompression surgery, and my body constantly is tight. My ‘natural’ state is tight, I hold my shoulders high, I have little stomach muscle putting all the strain on my back…I have nerve pain. I wake up feeling like I have been even tenser than I do when I’m aware of of tensing up. My body just aches … I was putting it down to ‘old age’. My only relief (and it doesn’t last long, about 3 hours)is swimming. I’m just exhausted.
I have learned that the main clenching comes from the anal muscles. If you relax those muscles and keep them relaxed it helps to over power the rest of the clenching in your body. Your article changed my life. I realized it’s your body’s natural fight or flight system and anxiety and other factors that make you learn how to take your body’s natural defense system and clench more then it would because in your mind you feel comfort. I clenched for years and realized that your anal muscles are the center of it all. I clenched real tight but I feel your brain naturally clenches these muscles when you have fear or anxiety and many other problems. Years of doing this caused pain all over because your pulling on all those muscle groups constantly. Ever since I relaxed the anal muscles and stayed aware of clenching those muscles that I have no more lower back pain, sciatic nerve pain and no more anxiety. Like you said this might not be everyone’s case but it helped me so much that I had to share my story because I know how depressing life can be with everything that comes with pain, stress, anxiety and more. This is coming from a person who grew up under intense stress and trauma. No medicine, therapy or anything else just learning to actually relax my muscles has changed everything. Stay focused and give it time you will start to feel better. I felt a big difference in the first few days and now months in I feel great.
I do this and with great intensity in my sleep. I recently clinched both knees so hard that I strained tendons in both knees. Three months and PT later, I am getting better. I wonder what will be my next area. Muscle relaxers make it worse.
This article describes me perfectly, I definitely am a chronic clencher and this peculiar bad habit of mine has given me a plethora of problems over the course of the years. Every single aspect of your description of global clenchers you can find on me, it’s terrific how accurate it is.
Due to a very large L5-S1 disc herniation – squats and sedentary lifestyle are the main culprits – I’ve recently developed Thoracic Outlet Syndrome and I’ve been reading a lot of your articles; trigger points, scapula positioning… Everything is as you say, I must have irritated my left brachial plexus by sitting with very poor posture (I also have strabismus, which doesn’t help) and by pulling my scapulas Up-Back and DOWN when doing dips for pecs. Among 3 neurosurgeons visited, only one diagnosed me correctly with it, but he just said to stop working out and go swim instead. Interestingly enough, I feel great relief by keeping the traps engaged and keeping the clavicles up. I’ve always had problems with squats, bench presses as I feel very weak doing them, despite being fairly strong on isolation exercises, and have frequently recurring external hemorroids as well. It all comes together… Very mildly myorelaxant benzodiazepines like low dose diazepam actually relieve the pain in my neck and make my arms feel extremely weak and fatigued, and that must be from all the clenching I unconsciously do. That’s crazy, I wish I could have a consult with you but unfortunately I live in Europe.
Thanks a lot for all your articles, they help a lot.
I broke my left big toe many years ago. I got a surgery and healed up and all was well save for some lack of mobility in that toe. Since then I’ve hurt it fairly bad a couple of times. The last time I ended walking with my toe flexed up towards the body while it healed. Now that it has healed, I cannot stop flexing that toe in the same manner every time I take a step. I do it even when sitting down but I can stop it upon realization there but I cannot stop it when walking. I believe this has caused pain and instability in my entire foot and all the way up to my knee.
Any suggestions other than don’t do it…which I don’t seem to be able to?
This is me. For almost 4 years I have lived in chronic pain from sciatic like symptoms and pudendal neuralgia. Therapy has never given me any relief, I knew there was something underlying all of this, something being missed. The pain began following several years of intense high stress situations and I mentioned it to every doctor but everyone ignored what I was saying. Thank you for publishing this!
I found this article because I am a chronic clencher and have been searching why I do this and what I can do to help myself. Not only do I tense my whole body but I also curl my toes and clench my hands where I’m constantly grabbing onto something. I do this while sleeping too. My leather steering wheel of my truck is all twisted from me constantly death gripping. I have been doing this since I was a small child as I’ve found numerous pictures of myself with my hands and feet clenched. I am not sure what it feels like to be relaxed. I am fully aware I’m clenching my muscles and I know I need to release them but I can’t. I get to the point where I get a lactic acid buildup and I start to feel like I’m burning. The only time I get some relief is when I take Aminos. A Dr diagnosed me with fibromyalgia 13 years ago but I know my clenching is a main cause of my discomfort. I just wish I could feel normal.
All of the characteristics in the above article apply to me. I have been a subtle body clencher my entire life, although I just realized it. At 43, I was diagnosed with severe fibromyagia with knots from .5 cm to 2.5 in all over my body.
I was unwilling to accept that there was no cause, so I started analyzing my muscle patterns. I started realizing that I clench my jaw, neck, back muscles, stomach, arm muscles, and, leg muscles when performing any movement. I also hold my breath constantly and even more during any movements.
I have tried to stop holding my breath but can’t figure it out. I have practiced diaphragmatic breathing but it causes severe rib pain under my left and right arms. Other therapists have given me instructions to not “turn on my neck” or “raise my shoulders” when I breath which lead to more clenching as I thought this meant to NOT use my scalenes to breath. Do you understand what this means, and are they correct?
Your articles state that the traps and scalenes SHOULD be working during breathing which feels far more normal to me. Am I understanding you correctly?
I also can’t meet lighter pressure for most movements. When I do feel a specific muscle, it is extremely difficult to exercise that muscle as I feel I lack the necessary stabilization for the rest of the body.
I know correcting pelvic, brachial, and cervical alignment are key, but I can’t figure out which to do first as my entire body seems to be the issue. Are there certain stabilizing muscles I should work and what order should I work them in?